Diagnosis
|
|||||
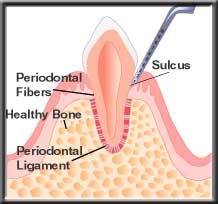 Healthy tooth |
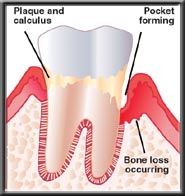 Bone loss leading to pocket formation |
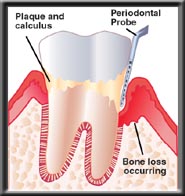 Using a probe to measure pocket depth and bone loss |
|
Each tooth is measured (probed) (See What is Periodontal Disease?) at six places, surrounding the tooth, to determine the pocket depth. Normally anesthesia is not needed for this charting, which gives the periodontist a blueprint of periodontal changes.
Other important information is collected during the examination, so an accurate diagnosis can be made.
- Gum recession - The amount of recession added to the pocket depth determines total bone loss.
- Furcations - Bone loss into the furcation (where the roots separate) of a tooth compromises the prognosis.
- Amount of attached gingiva - Without adequate attached gingiva, recession may occur.
- Occlusion (bite) - Excessive forces on teeth may increase the chances of bone loss.
- Tooth mobility (looseness) - Generally indicates inadequate bone support or a bite problem.
- Patient oral hygiene - Poor brushing and flossing will greatly compromise the long-term result.
Digital Dental Radiographs (X-RAYS)
A good series of dental x-rays is mandatory to accurately evaluate periodontal disease. They help determine the amount and location of bone loss, the size and shape of the roots, the amount of root still embedded in bone, the relationship of the teeth to each other, whether the nerve in a tooth has died, the location of the sinus and mandibular nerve when placing implants, and oral pathologies, among other things. We are not able to treat a patient unless we have adequate x-rays. The exception is gingival grafting, which normally does not require X-rays.
There are a number of different types of dental x-rays, each with a specific purpose, but for periodontal treatment a complete series of periapical films is generally required. Below is a list of the commonly taken x-ray views, and the indications for each.
- Full Mouth Periapicals - 16 - 18 detailed views of the teeth and surrounding bone, necessary for an accurate periodontal examination.
- Panograph - A single screening film showing an overview of the upper and lower jaws, sinus, temporomandibular joint, and other anatomic features.
- Bitewings - Four detailed views of the side and back teeth, primarily used to detect decay. Often used with the panograph by general dentists for routine new patient screenings.
- Vertical Bitewings - Four to seven detailed views of the teeth that can show both decay and bone levels when severe bone loss has not occurred.
- Digital X-rays - Any x-ray that is stored digitally, on a computer. Our X-rays are all digital.
Many people have a legitimate concern about the amount of radiation they receive with dental x-rays. It's un-nerving to watch the technician set the machine and run out of the room to expose the film! However, recent advances in dental x-rays make this an unnecessary concern. The film "speed" has improved dramatically, meaning that very little radiation is needed to expose the film. In fact, it is estimated that the amount of body radiation received with a complete mouth series is much less than one would receive at a day at the beach.
We now exclusively use digital X-rays which allows us to decrease the radiation to the lowest levels and results in higher image quality than ever before.
Diagnosis
Once the clinical data is gathered and correlated with the x-ray findings, we are able to organize and systematically evaluate the results to make a diagnosis. This is critical, for while there may be various approaches to treat a problem, there can be only one correct diagnosis. Once the diagnosis is determined, various treatment options can be formulated. With this information the periodontist and the patient can determine which treatment plan to follow.
 Click to View Larger |




 Detailed Diagnosis of Periodontal Disease
Detailed Diagnosis of Periodontal Disease